Cleidocranial Dysplasia (CCD) is a skeletal disorder characterized by open fontanelles (soft spot), small or absent clavicles (collarbones), and multiple dental abnormalities. It is a genetic birth defect caused by mutations to the RUNX2 gene. It occurs one in every one million births. It can be passed from an affected parent or can be a random mutation. Manifestations may vary among individuals in the same family.
Teeth
- Failure to lose baby teeth
- Failure for permanent teeth to come in on their own
- Supernumerary (extra) teeth
- Retention cysts
- Enamel hypoplasia: thin enamel caused by poor enamel formation
- Crowded teeth
- Jaw malocclusion: poor bite
Height
- People with CCD typically have a short stature
- Average height for men is 5’2″ – 5’6″
- Average height for women is 4’9″ – 4’10”
Head & Neck
- Delayed closure of fontanelles (soft spots)
- Large, open soft spot at birth that may close or remain open throughout life
- Parietal bossing (broad/flat forehead)
Chest
- Narrow thorax (chest)
- Ability to touch shoulders together
- Small scapula
- Small or absent clavicles (collarbones) with sloping shoulders
- Short ribs
- Cervical ribs: extra ribs that arise from vertebrae in the neck
Face
- Small mid-face: the portion of the face comprising nasal (nose), maxillary (upper jaw), and zygomatic bones (cheekbones) and the soft tissues covering these bones
- Frontal bossing: prominent, protruding forehead
- Metric groove: vertical dent in the middle of the forehead, normally not present at birth
- Micrognathia: small lower jaw
Skull
- Wormian bones: extra bone pieces that occur within the joints of the cranium
- Bossing (protruberance) of frontal bone
- Bossing of occipital bone
- Bossing of parietal bone
- Calvarial (skull) thickening
- Absent or small frontal sinuses
- Absent or small paranasal sinuses
- Large foramen magnum: the hole at the base of the skull through which the spinal cord passes
Spine
- Spondylolysis: a defect in the vertebral arch in the lumbar or cervical vertebrae
- Spondylolisthesis: a condition where one vertebral body is slipped forward over another
- Scoliosis: a lateral curve in the spine
- Kyphosis: a curve in the spine that results in a bulge at the upper back
Pelvis
- Wide pubic symphysis (the joint in the pubic bone)
- Delayed mineralization of pubic bone
- Broad head of the femur bone
- Short neck of the femur bone
- Coxa vara: hip deformity where the head and shaft of the femur is reduced to less than 120 degrees, resulting in a short leg and a limp
- Underdeveloped iliac wing (pelvic bone)
Hands
- Brachydactyly: short fingers
- Long second metacarpal (hand bone)
- Short middle bones of second and fifth fingers
- Cone-shaped finger tips
- Short and broad thumbs
Legs
- Gene valgum: a condition in which knees are deviated towards midline of the body and touch one another when the legs are straightened (“knock knee”)
Legs
- Gene valgum: a condition in which knees are deviated towards midline of the body and touch one another when the legs are straightened (“knock knee”)
Ears
- Deafness
Eyes
- Hypertelorism: increased distance between the eyes
Nose
- Low nasal bridge
Mouth
- Narrow, high-arched palate (roof of mouth)
Respiratory
- Respiratory distress in early infancy
Skeletal
- Osteopenia: reduced bone mass. Increased bone fragility
Feet
- Lower or flattened arches in the feet
Neurologica
- Syringomyelia: fluid-filled cysts in the spinal cord
How is CCD diagnosed?
Physical Exam & Clinical Findings
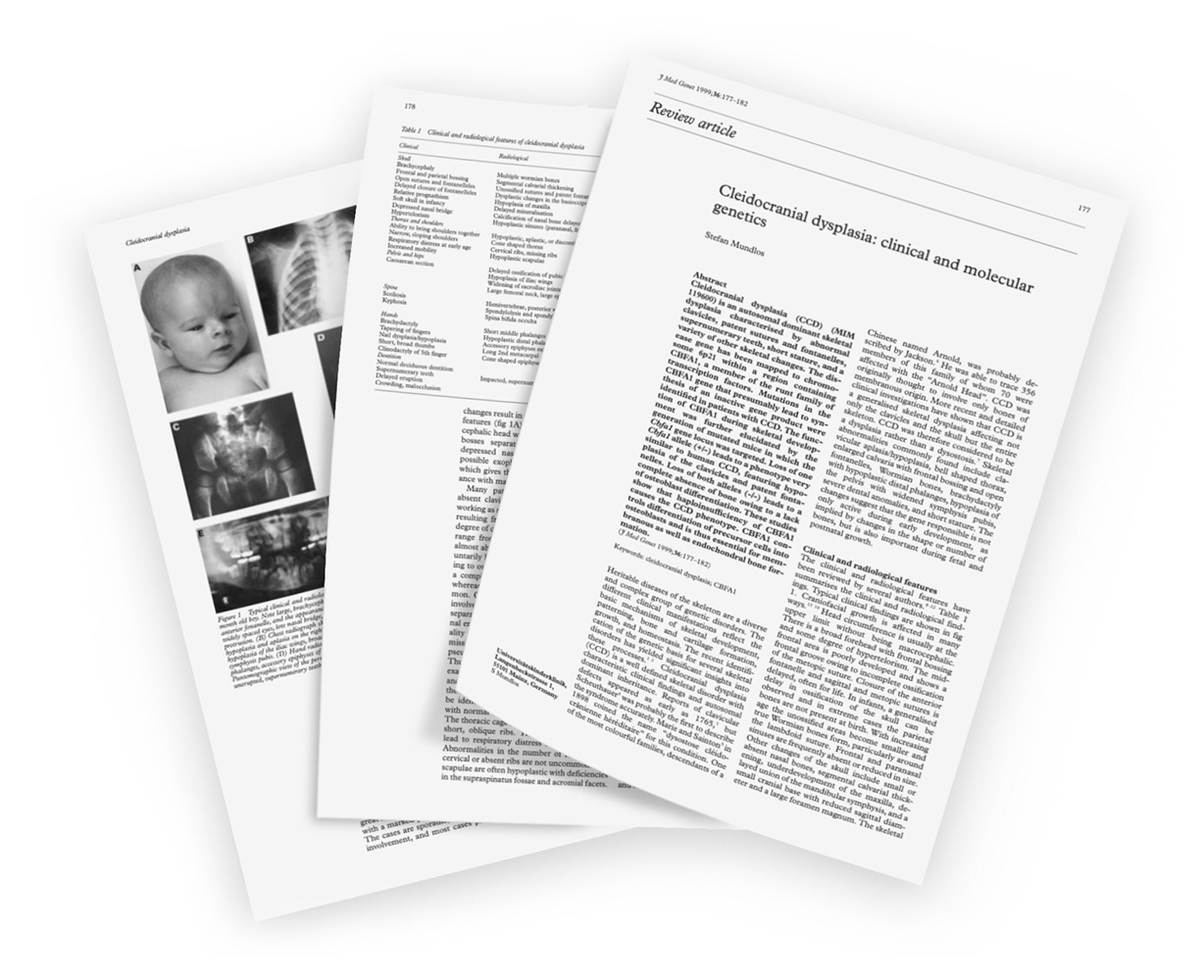
CCD can be diagnosed by they “characteristic triad” of small or absent clavicles, open fontanelles (soft spot), and supernumerary (extra) teeth. Other clinical findings include small mid-face, abnormal teeth, hand abnormalities, normal intellect
X-Ray Findings
Skull: wide or open fontanels (soft spot), presence of wormian bones; delayed bone formation; poor development of paranasal, frontal or mastoid sinuses; crowded or extra teeth. Chest: narrow thorax, small or absent clavicles, small scapulae. Pelvis: wide symphysis pubis, small pelvic bones, wide sacroiliac joint, short femoral neck. Hands: long second metacarpal, underdeveloped distal finger bones, cone-shaped finger tips.
Genetic Testing
The test looks for changes in the RUNX2 gene. The gene is found 60-70% of the time in people with a clinical diagnosis of CCD. Prenatal diagnosis can be made by ultrasound examination in offspring of affected parent as early as 14 weeks.
Other medical conditions seen in individuals with CCD
- Recurrent sinus infections
- Upper-airway complications
- Recurrent ear infections
- High incidence of cesarean section
- Mild degree of motor delay in children under age five years
- Fine-motor skills (grasping a pencil, using a spoon)
- Gross-motor skills (walking, hopping, climbing stairs)
Other conditions that share characteristics with CCD
- Congenital psyeduoarthrosis of the clavicle
- Pyknodysostosis
- Crane-Heist syndrom
- Manibuloacral dysplasia
- Yunis-Varon syndrome
- Hypophosphatasia
- CDAGS syndrome
- Parietal foramina with cleidocranial dysplasia
Children with CCD should be monitored for the following
- Orthopedic complications
- Dental abnormalities
- Upper-airway obstruction
- Hearing loss
- Osteoporosis
What causes CCD?
Humans have 23 pairs of chromosomes. 22 pairs are called autosomes the 23rd pair, the sex chromosomes, differ between males and females. Humans have about 20,000 functioning (or protein coding) genes, found on the 23 chromosomes.
Humans have two of each gene, one from mother and one from father. If your parents each give you matching genes, they are called homozygous. If the genes are different from each other, they are called heterozygous. A mutation is the changing of the structure of a gene. When one gene has less or no function, it is called a loss-of function mutation. The gene causing CCD is the RUNX2 gene and is found on the 6th chromosome. The 6th chromosome has 1,048 protein coding genes, the RUNX2 gene is one of these.
Cleidocranial dysplasia (CCD) is caused by heterozygous loss-of-function mutation in the RUNX2 gene on the 6th chromosome. The mutation to the one gene can be: 1) passed from an affected parent 2) can be a new or random mutation.
CCD is an autosomal dominant trait. This means the gene affected is on an autosome (one of the 22 pairs of chromosomes that is not the sex chromosome). It only takes a single abnormal gene (not an abnormal chromosome) from either parent to cause an autosomal disorder.A dominant trait means an abnormal gene from one parent can cause the disease. This happens when the matching gene from the other parent is normal. The abnormal gene dominates. A parent with an autosomal dominant conditions has a 50% chance of having a child with the condition. This is true for each pregnancy (Each pregnancy is a 50/50 chance. The child’s risk for the disease does not depend on whether their sibling has the disease).
Timeline & Evolution of CCD
The main clinical features of CCD include persistently open fontanels (soft spots) with bulging skull, underdeveloped or absent of the clavicles (collarbones), wide pubic symphysis (the joint of the pubic bones), short middle phalanx (bone) of the fifth fingers, dental anomalies, and often vertebral (bones of the spinal column) abnormalities.
1765
Reports of the defect first appeared.
1898
Coined dysostose cleidocranienne hereditaire or cleidocranial dysostosis.
1909
Skeleton of a 25 year-old man showed underdeveloped clavicles, open anterior soft spot, and touching knees (genu valgum).
1951
356 descendants were traced to the Chinese man Arnold, 70 of whom were affected with the “Arnold Head.” He lived in South Africa and had 7 wives.
1976
Reported a family with delayed eruption of baby and permanent teeth, probably CCD.
1987
Described association of CCD and syringomyelia (fluid-filled cysts in the spinal cord).
1987
Proposed the gene symbol “CCD”. Studied CCD in mice and found the homozygous (2 mutated RUNX2 genes) state in mice was lethal.
1990
Height and radius length are decreased, especially in females. CCD is a generalized skeletal dysplasia.
1992
Described the range of variability in affected members in 3 generations of family.
1993
Concluded that under formation of the hyoid bone could be added to the delayed process of bone formation that affects the skull, teeth, pelvis, and extremities.
1993
Proposed that CCD gene is located on chromosome 6.
1995
The CCD gene was assigned to chromosome 6 ( 6p21).
2001
Found the following complications that had previously been unrecognized: genu valga (knock-knee), scoliosis, pes planus (flat foot), sinus infections, upper respiratory complications, recurrent middle ear infections and hearing loss. Primary rate of c-sections was increased. Dental abnormalities: extra teeth, failure to lose baby teeth, abnormal jaw alignment.
2002
Mutation causes abnormalities due to defective mineralization.
2002
Osteopenia, osteoporosis and decreased alkaline phosphatase likely occur in a minority of patients with CCD.
2005
Humans with CCD have altered endochondral bone formation (where process where bones grow in length, where cartilage turns to bone).
2005
Sequenced the RUNX2 gene and identified 12 RUNX2 mutations. They observed mild to full-blown expression of the CCD characteristics, with variability in families.
2010
RUNX2 appears to play a role in the formation of bone and bone cell differentiation.